Verification is just checking if they are "Active." Elva gets you a Breakdown. It is the only autonomous agent that secures your revenue by predicting denials before they happen, handling everything from Edge Case verification to writing clinical appeals when payers try to bundle your procedures.

Automated Benefit Verification
Autonomously verifies benefits before arrival. Patients know exact copays, stopping surprise bills at the front desk.
99% First-Pass Claim Rate
Elva builds rejection-proof claims by checking codes and notes, ensuring you get paid on the first try every time.
Automated Denial Recovery
Turn dead revenue into cash. Elva investigates rejections and executes appeals to recover funds staff often write off.
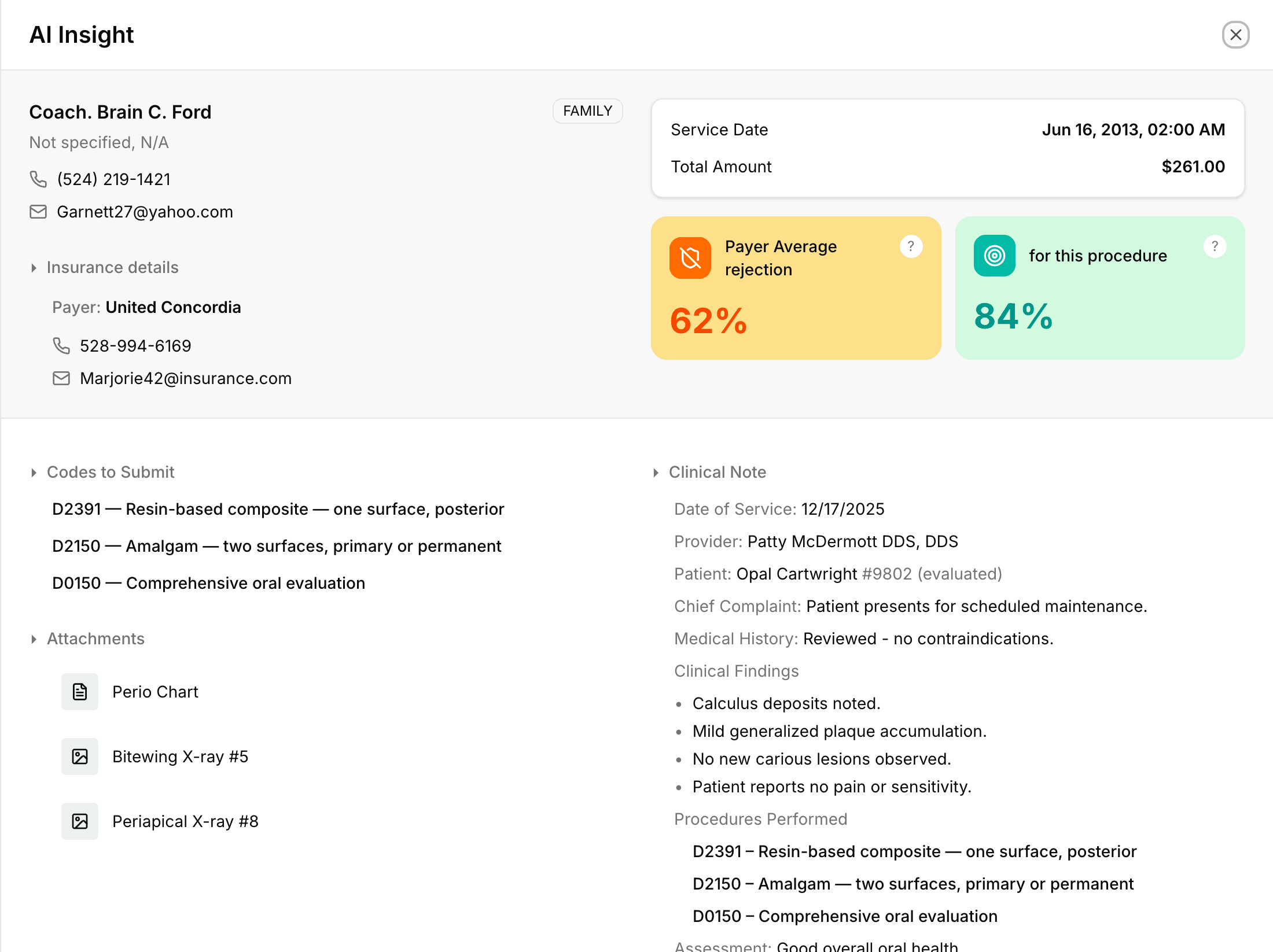
The "Insight" Script
Generates a "Morning Huddle" whisper for your front desk, highlighting exact financial risks and talking points.
Eliminate the "Surprise Bill" Conversation Forever
Nothing kills a 5-star patient experience faster than an unexpected bill at the front desk. Elva works ahead of your schedule, automatically verifying full benefit breakdowns, remaining deductibles, and exact copays days before the patient walks in. This means your team stops wasting hours on hold with insurance carriers and starts having confident, transparent financial conversations. Patients arrive knowing exactly what they owe, eliminating awkward arguments and ensuring you collect 100% of the patient portion at the time of service.
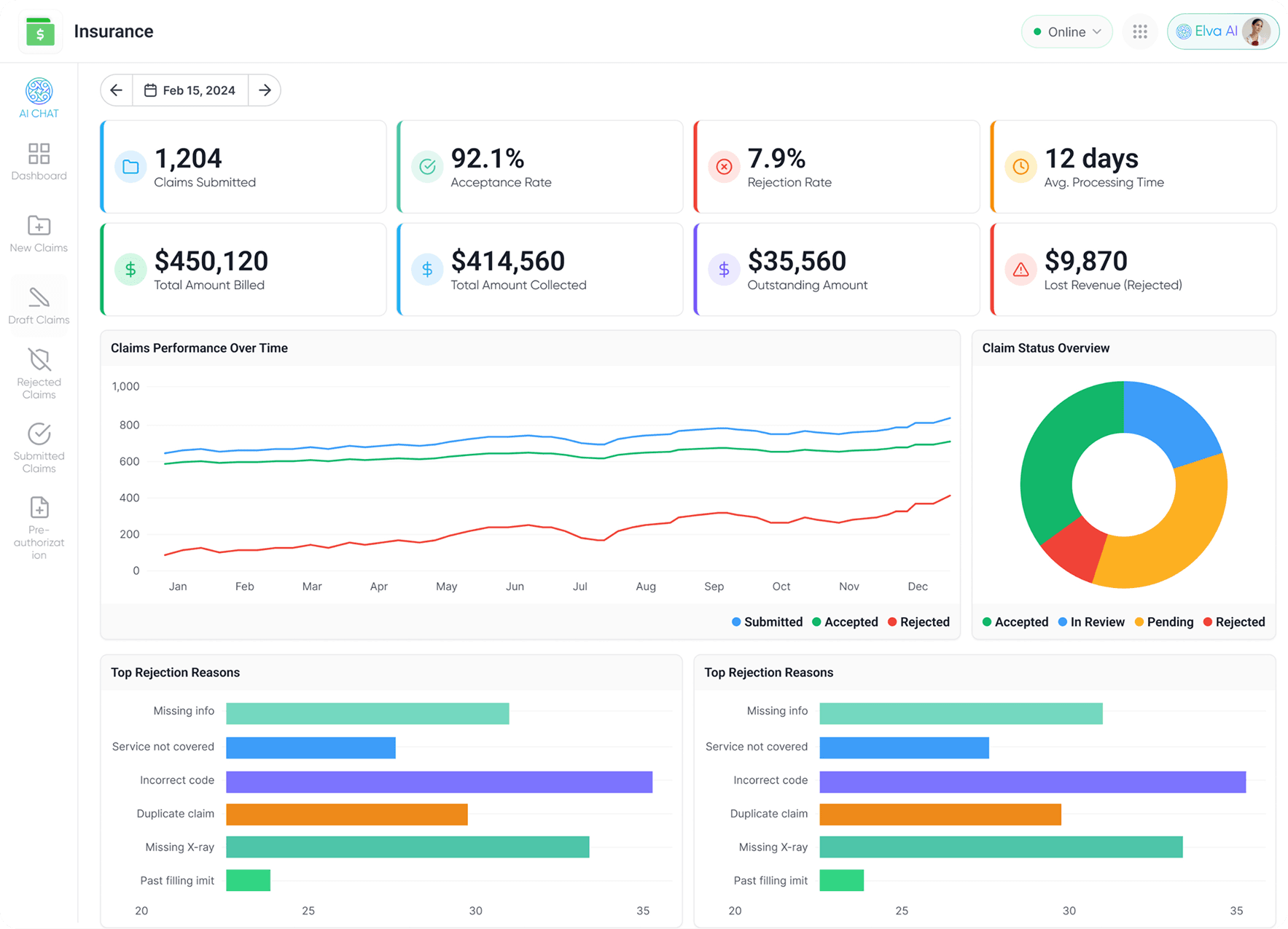
Stop Fighting Rejections and Get Paid on the First Try
Submitting claims shouldn't feel like a gamble. Elva acts as your expert biller, proactively cross-referencing every procedure code, clinical note, and required attachment (like X-rays and perio charts) against the specific rules of that payer. It builds a "rejection-proof" claim package that is designed to get approved the first time. Stop spending your week chasing denials or fixing simple clerical errors. With Elva, you get paid faster, keep your cash flow healthy, and liberate your staff from the "shackles of administrative burden" so they can focus on patient care.
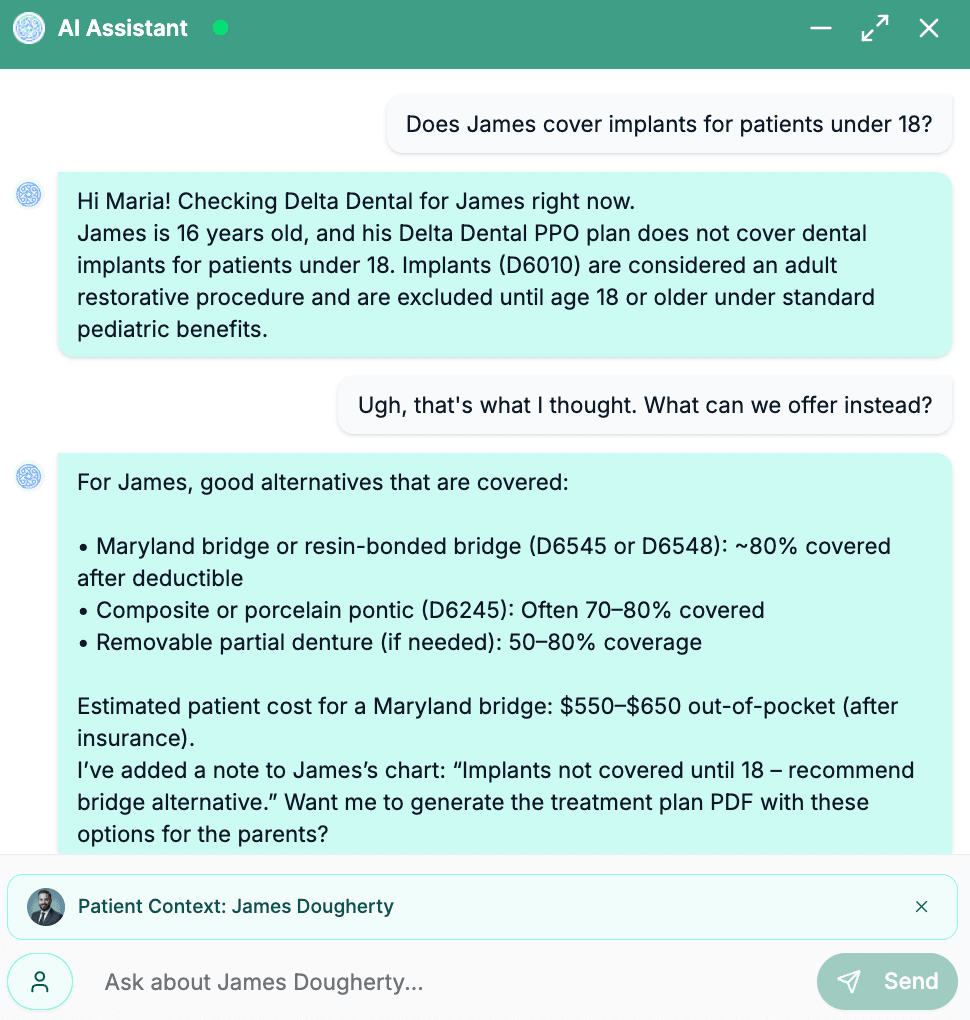
Chat Directly With Your Insurance Data
Sometimes you don't need a report; you need an answer. With Elva, you can chat directly with your insurance data. Ask complex questions like "Does Aetna cover implants for patients under 18?" or "Show me all claims from last month denied for 'Medical Necessity'." Elva instantly scans your entire database and payer rules to give you a clear, plain-English answer, acting as a 24/7 consultant for your toughest billing questions.
Your Team Is for Care. Elva Is for Claims
Experience the peace of mind of a revenue cycle that runs itself 24/7/365.
Your AI Insurance Workforce Is Ready to Get Started
Elva autonomously handles eligibility, coding, submissions, authorizations, denials & A/R, ensuring faster payments, near-zero rejections, and predictable cash flow.

Never Worry About an Eligibility Check Again
Elva knows your schedule. It doesn't wait to be told; it proactively and autonomously verifies every patient at the right time. Your team gets 100% accurate, up-to-date benefits for every check-in.

Make Every Claim "Audit-Proof" on Autopilot
Elva is your 24/7 compliance manager. It actively reviews your clinical charts and codes as they're written, flagging inconsistencies that trigger denials and protecting your practice.

Let Elva's AI Manager Appeal Your Denials
Elva is your expert biller. It investigates the rejection, gathers the evidence, and executes the appeal process to recover the money you are owed.

Let Elva Autonomously Secure Your High-Value Treatments
Stop letting revenue stall. Elva's AI reads your treatment plans, knows which procedures require pre-auth, and autonomously manages the entire submission and follow-up.

Elva’s AI Builds Your Rejection-Proof Claims
Elva builds the perfect claim package for your team to review. It gathers the right notes, flags the right codes, and attaches the right documentation for 99% first-pass approval.

Put Your Insurance A/R on Autopilot
Stop letting old claims die. Elva's AI is your tireless A/R manager, working your aging insurance claims 24/7. It autonomously follows up, checks status, and pushes claims toward payment.
Elva isn't just an insurance checker. It's your versatile strategist.
Advanced workflows that handle the complex administrative burdens of billing, from clinical coding to payment posting.
Insurance Benefit Maximizer
Don't let benefits go to waste. Elva identifies patients with unused benefits in Q4 and prompts them to book pending treatment before the "Use It or Lose It" deadline resets their deductible.
Smart Cost Estimation
Elva calculates the exact "Patient Portion" by accounting for downgrades (like Composite to Amalgam). It gives patients a transparent, accurate estimate, reducing billing disputes.
Accounts Receivable Automation
Elva relentlessly follows up on aging claims. It prioritizes high-value unpaid claims and contacts the payer, reducing your Days Sales Outstanding (DSO) automatically.
Private Data Silos for DSOs
For large groups, Elva ensures that insurance and patient data is kept secure and local, respecting strict data governance and HIPAA requirements.
Stop Playing Games with Insurance Companies
Stop letting insurance companies dictate your revenue. Equip your practice with the AI that knows their rules better than they do.
Schedule a Demo