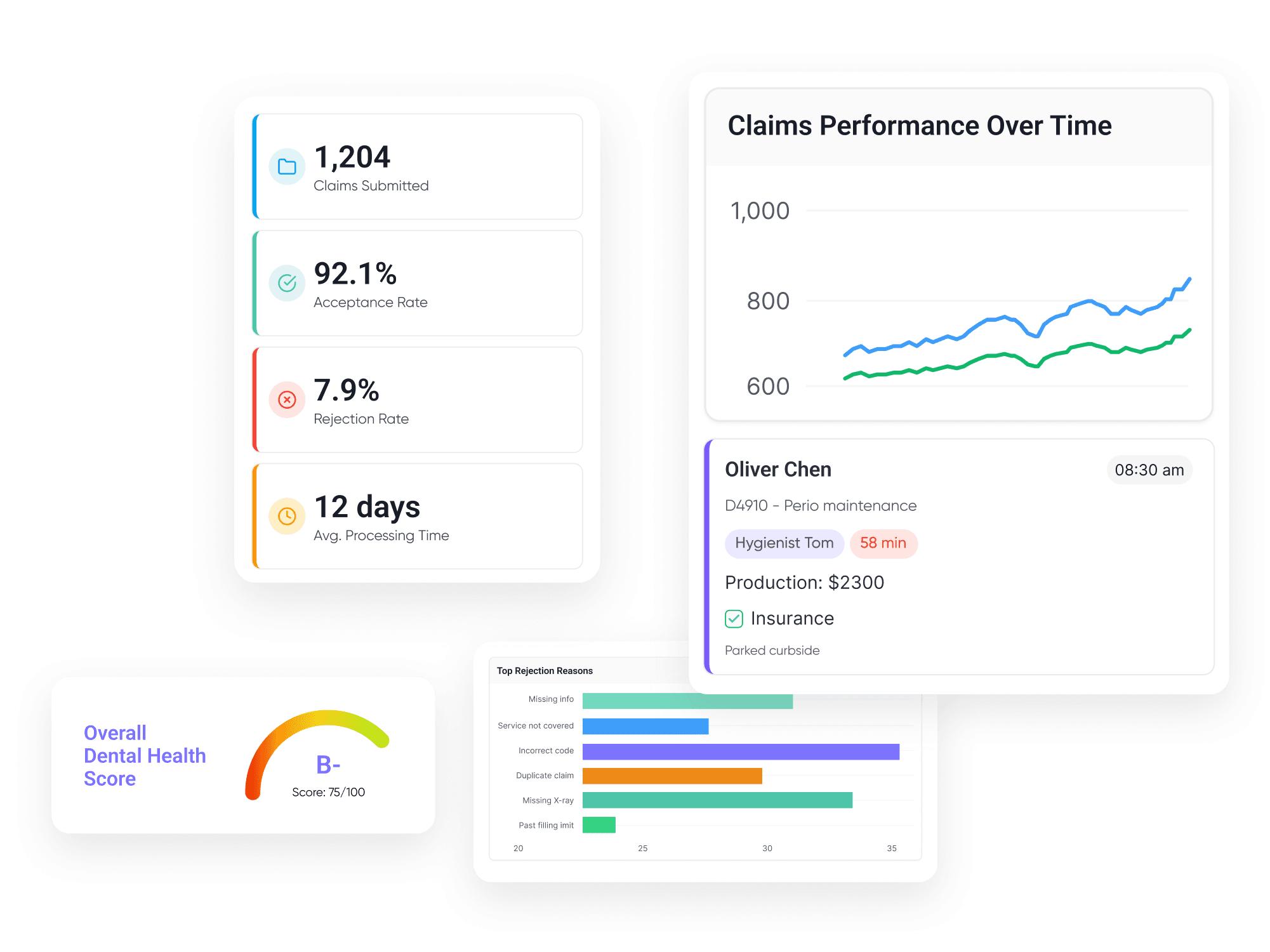
Secure Approvals for High-Value Cases Without the Wait
Elva automates the entire authorization lifecycle. It identifies procedures requiring approval, compiles the clinical evidence (X-rays, charts, narratives), submits the request, and tracks it daily, so you never have to sit on hold with a payer again.
Auto-Identification
Instantly flags CPT/CDT codes that require Pre-Auth based on the specific payer's rules.
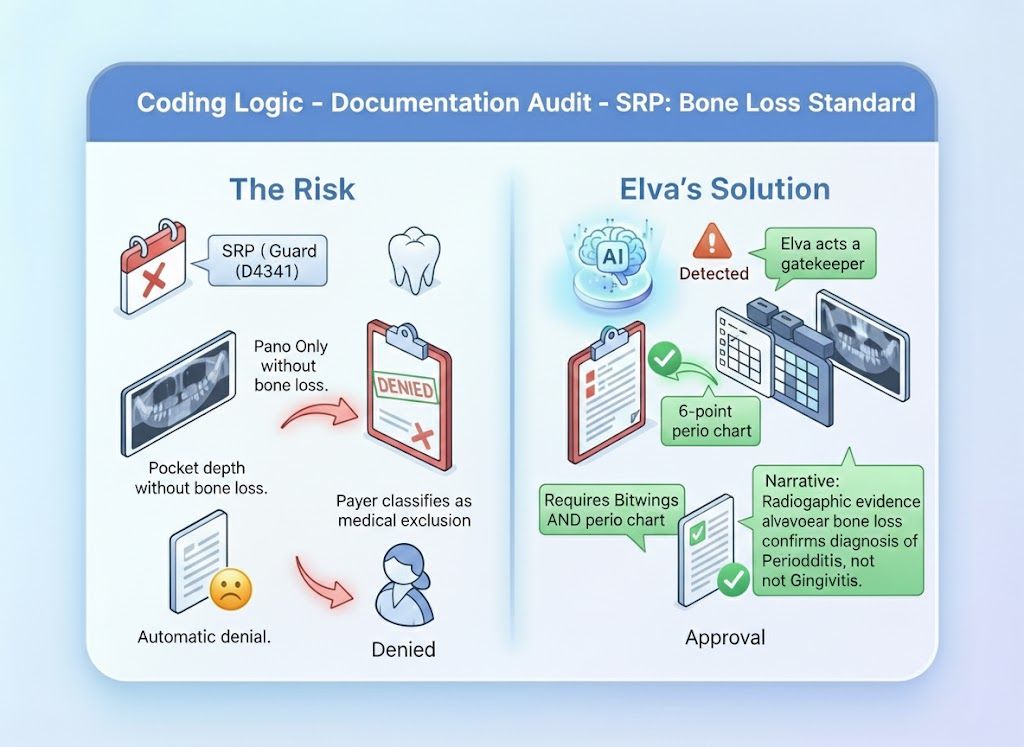
Evidence Compiler
Autonomously pulls the exact Perio Chart, PA X-ray, or Photo required to prove medical necessity.
Status Watchdog
Pings the payer portal daily to check status, alerting you the moment an approval (or denial) drops.
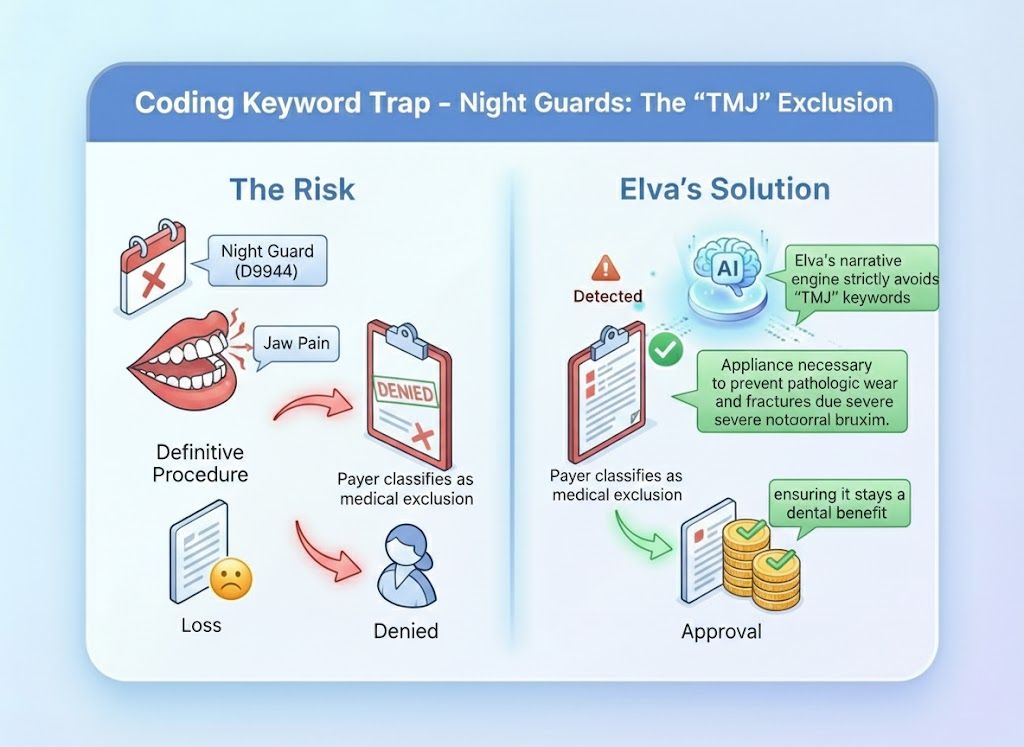
Narrative Generator
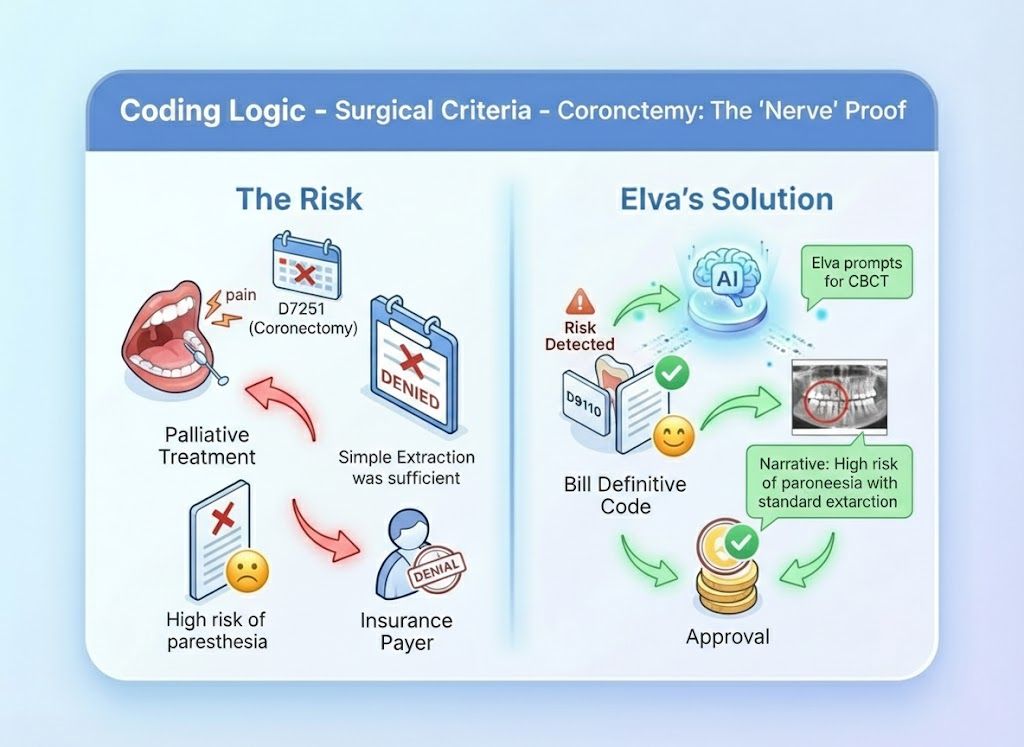
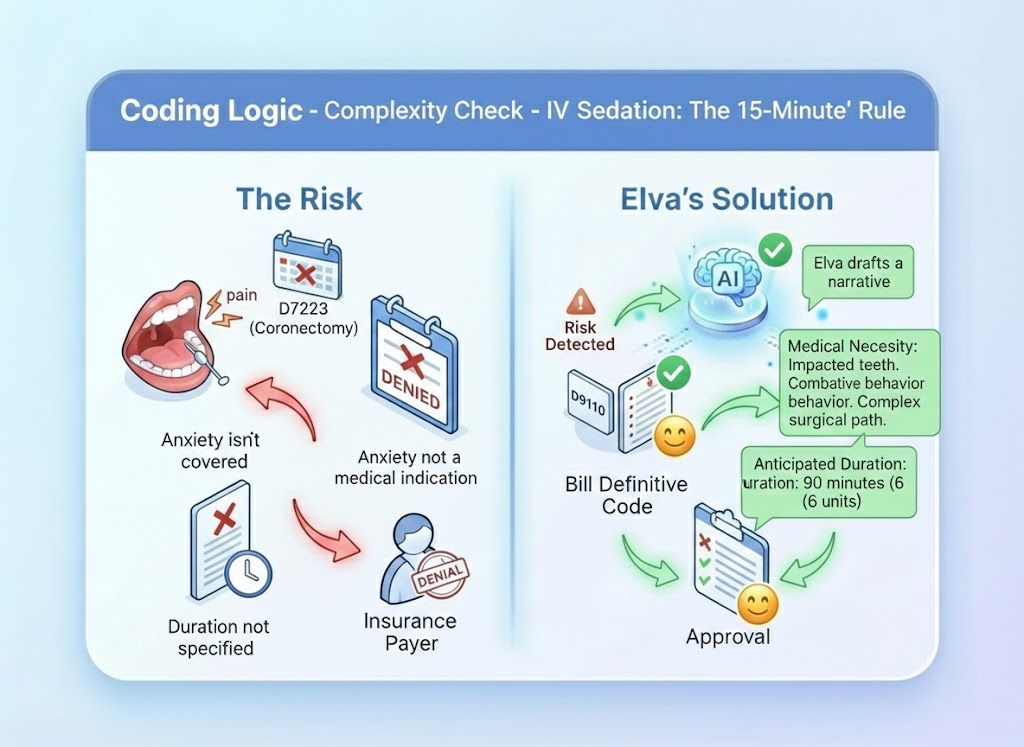
Writes clinical narratives using "Gold Standard" keywords that trigger approval algorithms.
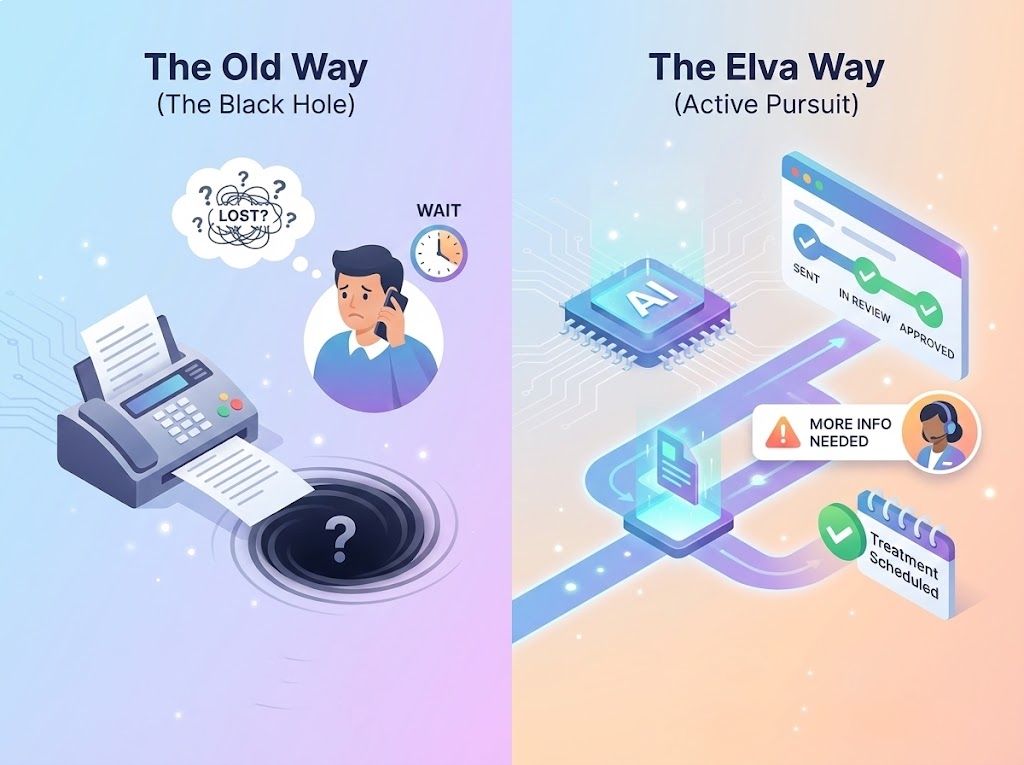
The "Fax Black Hole" vs. Digital Transparency
The Old Way (The Black Hole): You fax the request and wait. And wait. You have no idea if they received it, if it’s being reviewed, or if it’s lost. You have to call 3 times just to get a status update, delaying treatment for weeks. The Elva Way (Active Pursuit): Elva submits digitally and tracks the claim like a package. It updates the status in your PMS (e.g., "Sent," "In Review," "Approved") daily. If the payer asks for "More Info," Elva alerts you instantly so you can fix it that same day.
Don't check the portal. Just ask.
Your team can check the status of a case instantly or ask what is required for a specific submission. Dr. Smith: "What's the status of the Pre-Auth for Sarah Jones' Implant?" @Elva: Status: APPROVED. Received today. Valid through Dec 31st. Note: They approved the Implant (D6010) but denied the Ridge Augmentation (D7953). I have uploaded the approval letter to the Document Center."

"Pending" is Not a Strategy
Waiting 30 days for a letter that might say "Denied" kills your case acceptance. Elva speeds up the clock by submitting a "Perfect Packet" the first time, cutting turnaround time by weeks.
Automated Authorization Workflow
From the moment you diagnose treatment, Elva takes over the paperwork, ensuring you have the "Green Light" before you pick up the scalpel.

One-Click Submission
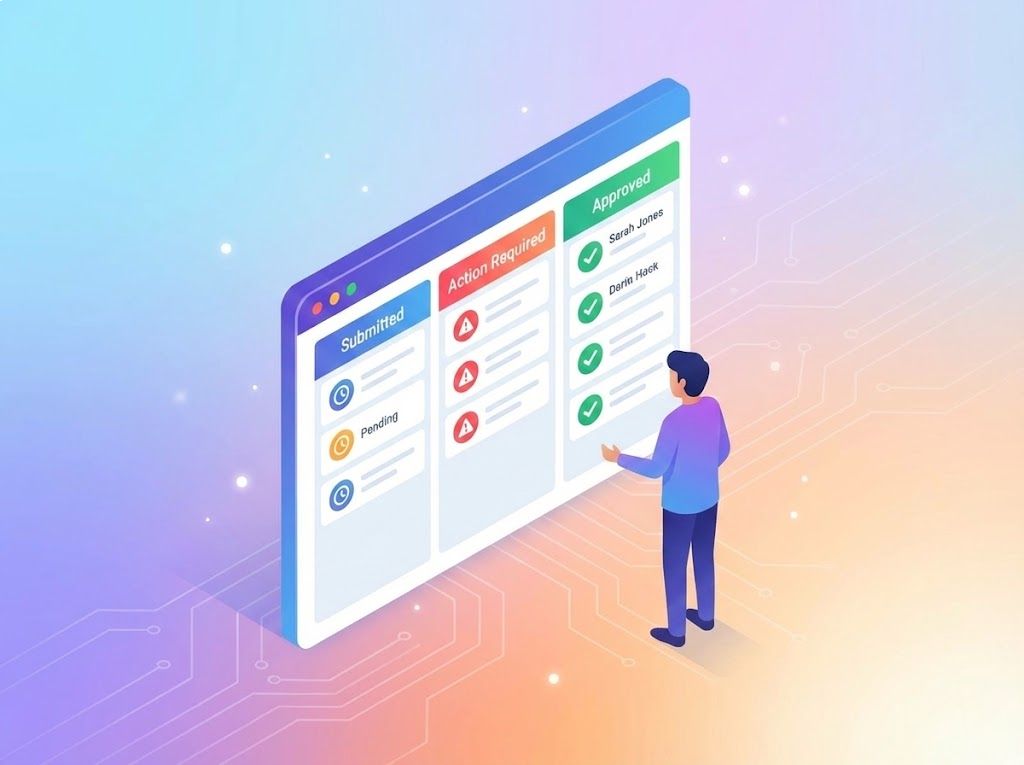
Real-Time Status Dashboard
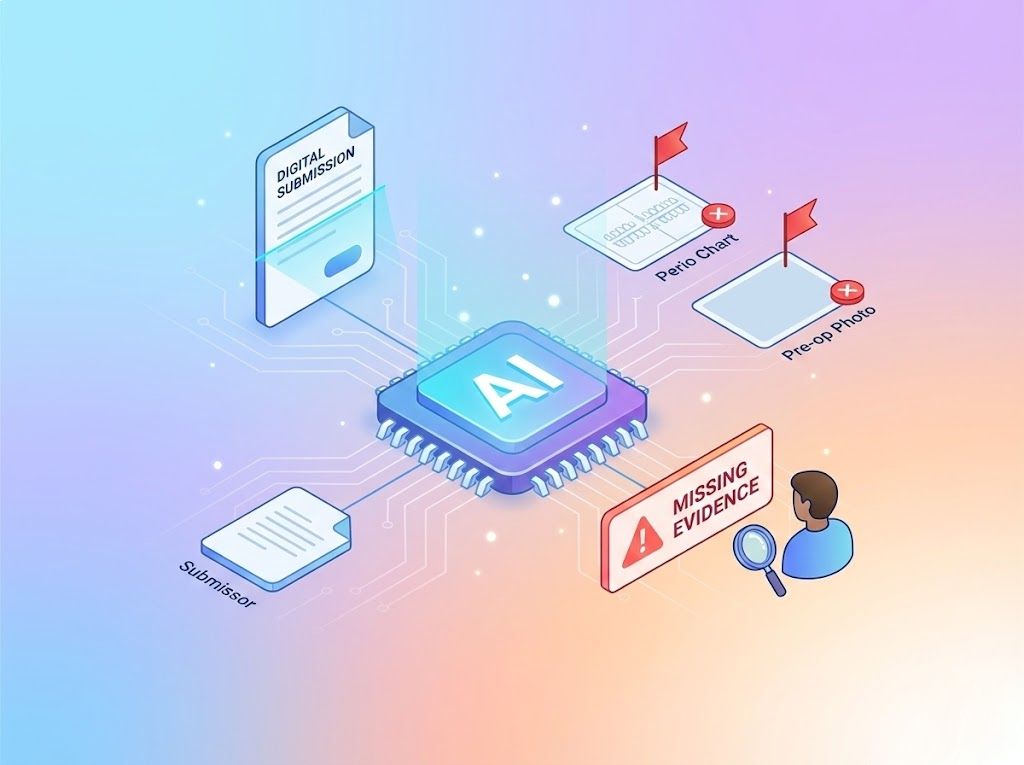
Clinical Gap Analysis

Patient "Green Light" Texting
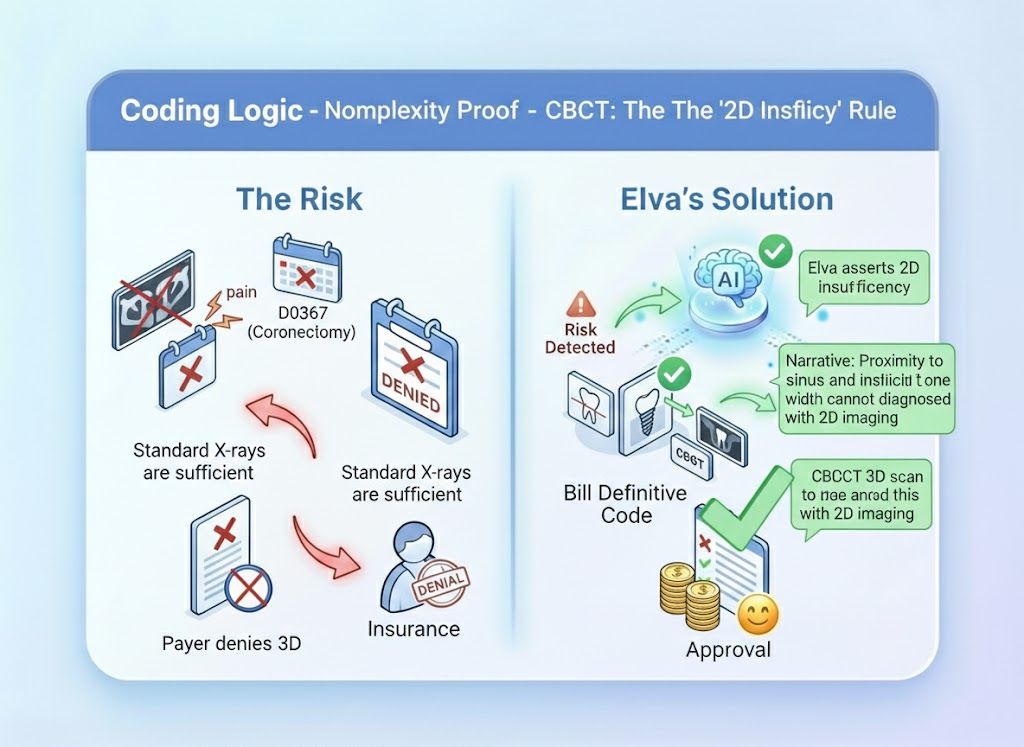
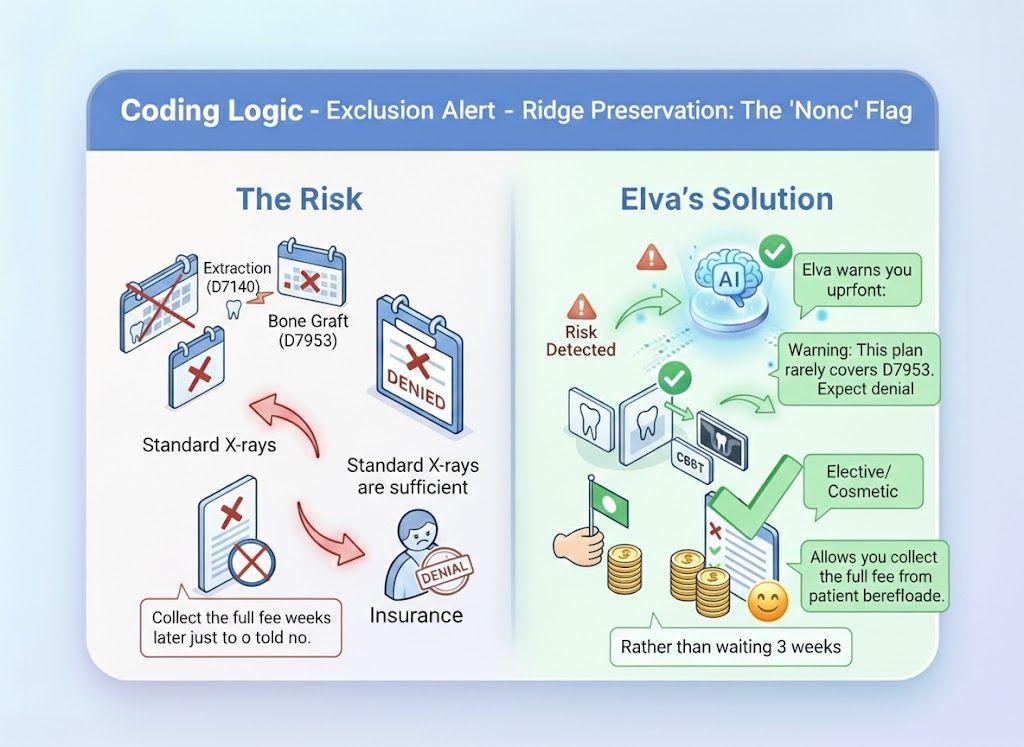
The "Medical Necessity" Proof Engine
Payers look for reasons to deny expensive procedures. Elva knows the exact clinical criteria, from "nerve proximity" to "bone loss measurements", that adjudicators need to see to say "Yes."
Get the "Yes" Before You Prep
Stop letting administrative delays bottle-neck your production. Submit perfect Pre-Auth packets that payers can't refuse.
Schedule a Demo